Examining Youth Mental Health Symptom Levels Before and During the Pandemic: Implications for Health Care Delivery Systems
Key Message
Youth patients screened during COVID-19 exhibited significantly higher symptoms of depression, anxiety, and PTSD compared to youth patients screened pre-COVID-19.
Abstract
Authors
Jessica Kay Jeffrey, MD, MBA, MPH; Wendy Barrera, MPH; Hilary Aralis, PhD; Rachel Linonis, MS; Mark Grossman, MD, MBA; Patricia Lester, MD
Objective
This poster examines data from UCLA Behavioral Health’s (BHA) Collaborative-Pediatric Primary Care program spanning 2018-2022, revealing concerning trends of elevated youth mental health symptom severity for patients at intake during the pandemic.
Methods
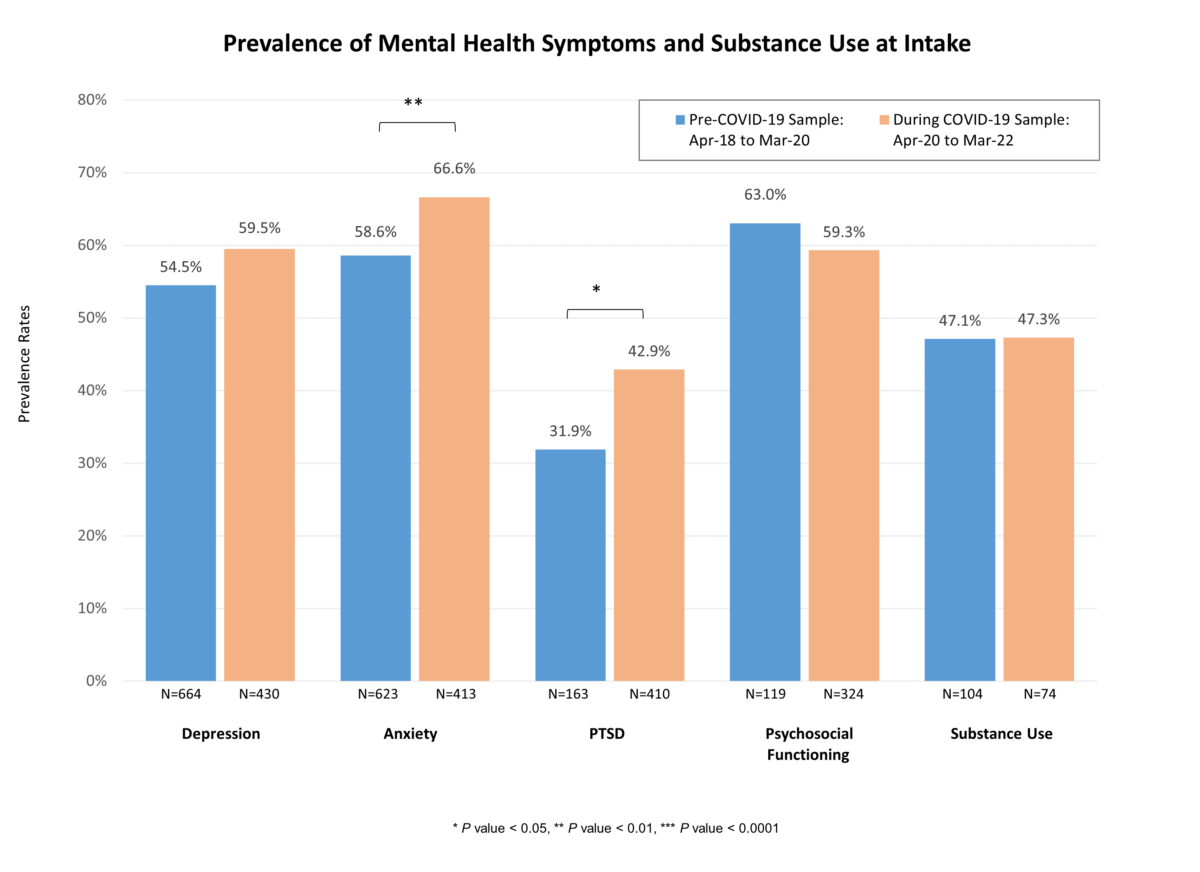
A convenience sample of data collected from April 2018 to March 2020 across BHA were analyzed. We compared the mental health symptoms and substance use of a population of 668 youth patients at their intake screening prior to COVID-19 (April 2018 to March 2020) versus a population of 441 youth patients at their intake screening during COVID-19 (April 2020 to March 2022). Depression, anxiety, PTSD, psychosocial functioning, and substance use were assessed using the Mood and Feelings Questionnaire – Short Form (MFQ-SF), Screen for Child Anxiety Related Disorders (SCARED), Child PTSD Symptom Scale (CPSS), Pediatric Symptom Checklist – Youth (PSC-Y), and CRAFFT, respectively. The hypothesis that youth patients experienced higher levels of mental health symptom severity and substance use during COVID-19 was examined using independent samples t-tests to compare differences in symptoms and substance use prior to versus during COVID-19.
Results
Youth patients screened during COVID-19 exhibited significantly higher symptoms of depression, anxiety, and PTSD compared to youth patients screened pre-COVID-19 (all p < 0.05). Although not statistically significant, youth patients screened during COVID-19 reported lower symptoms of psychosocial functioning and substance use. Additionally, they attended a significantly greater number of therapy and physician visits (both p < 0.01).
Table 1: Mean Mental Health Symptoms and Substance Use at Intake
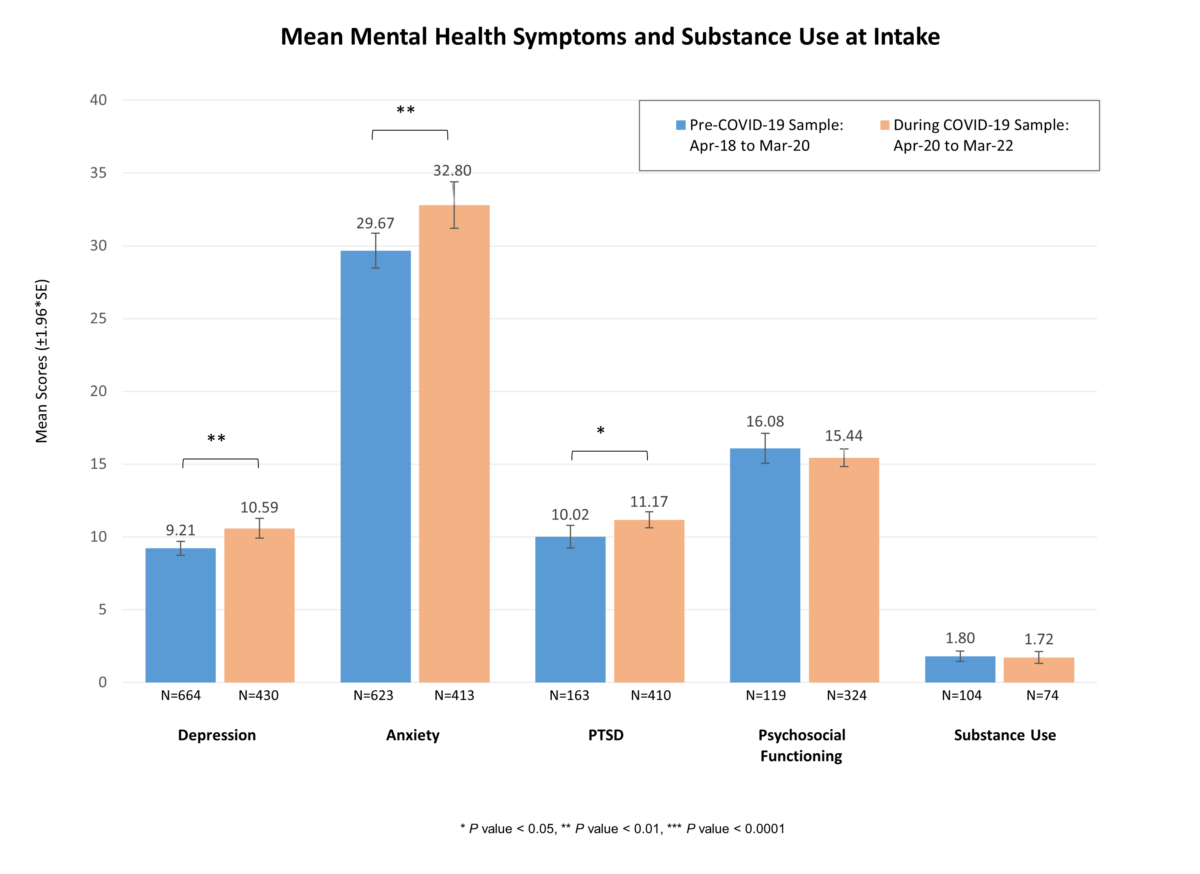
Table 2: Prevalence of Mental Health Symptoms and Substance Use at Intake
Conclusions
Data from UCLA BHA’s Collaborative-Pediatric Primary Care program spanning 2018-2022, reveals concerning trends of elevated youth mental health symptom severity and psychosocial functioning during the COVID-19 safer-at-home restrictions. Highlighting the urgency of the situation, the poster emphasizes the immediate need for attention and action to address the worsening youth mental health crisis. To effectively address youth mental health needs, the development and implementation of robust information systems that comprehensively address the complex needs of youth mental health is recommended. This entails enhancing screening, intervention, and overall support for youth mental health.
Taking Action
In the 2021 report “Protecting Youth Mental Health: The U.S. Surgeon General’s Advisory,” the U.S. Surgeon General recommends that care systems rethink how it deals with youth mental health. This involves:
- Prioritizing prevention as the most effective treatment for mental health challenges.
- Regularly screening young individuals for mental health issues and risk factors, including Adverse Childhood Experiences (ACEs).
- Recognizing and addressing the mental health needs of parents, caregivers, and other family members.
- Collaborating between clinical staff and trusted community partners and child-serving systems (e.g., child welfare, juvenile justice).
- Establishing multi-disciplinary teams to provide tailored services for children and their families.
References & More Reading
- Cifuentes, M., Davis, M., Fernald, D., Gunn, R., Dickinson, P., & Cohen, D. J. (2015). Electronic health record challenges, workarounds, and solutions observed in practices integrating behavioral health and primary care. Journal of the American Board of Family Medicine: JABFM, 28(Suppl 1), S63–S72. https://doi.org/10.3122/jabfm.2015.S1.150133
- Mental Health America. (2023). The state of mental health in America. https://mhanational.org/issues/state-mental-health-america
- Office of the Surgeon General (OSG). (2021). Protecting youth mental health: The U.S. Surgeon General’s advisory. U.S. Department of Health and Human Services. https://pubmed.ncbi.nlm.nih.gov/34982518/
- The White House. (2023, February). White House report on mental health research priorities. https://whitehouse.gov/wp-content/uploads/2023/02/White-House-Report-on-Mental-Health-Research-Priorities.pdf
- Weisz, J. R., Sandler, I. N., Durlak, J. A., & Anton, B. S. (2005). Promoting and protecting youth mental health through evidence-based prevention and treatment. American Psychologist, 60(6), 628–648. https://doi.org/10.1037/0003-066X.60.6.628